Health
Biologics: Transforming Treatment for Autoimmune Diseases
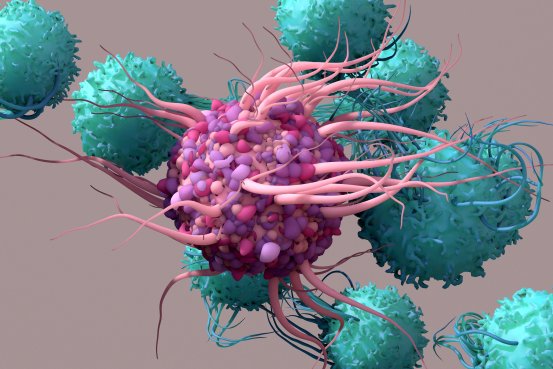
Millions worldwide suffer from autoimmune diseases such as psoriasis and rheumatoid arthritis. Biologics and biosimilars have revolutionized treatment by modulating the immune system, alleviating symptoms, and improving patients’ quality of life.
Millions worldwide suffer from autoimmune diseases such as psoriasis and rheumatoid arthritis. Biologics and biosimilars have revolutionized treatment by modulating the immune system, alleviating symptoms, and improving patients’ quality of life.
Understanding Autoimmune Diseases and Their Effects on the Skin
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues and organs. These disorders can affect multiple systems, including the skin, producing a wide range of dermatological manifestations that can significantly impact daily life.
1. Common Autoimmune Skin Conditions
Several autoimmune diseases primarily target the skin:
-
Psoriasis: Characterized by raised, scaly, and often itchy patches.
-
Lupus: May cause a butterfly-shaped facial rash and other skin lesions.
-
Scleroderma: Leads to thickening, hardening, and tightening of the skin.
-
Dermatomyositis: Presents with muscle weakness accompanied by distinctive skin rashes.
2. The Role of Biologics in Treatment
Biologics are medications derived from living organisms. Unlike traditional drugs, they target specific components of the immune system to reduce inflammation, prevent further tissue damage, and control disease progression. Biologics are often prescribed when conventional treatments fail to provide adequate relief.
3. Types of Biologics Used for Skin Conditions
Commonly prescribed biologics include:
-
TNF-alpha inhibitors: Etanercept, adalimumab, infliximab
-
IL-17 inhibitors: Secukinumab, ixekizumab
-
IL-23 inhibitors: Guselkumab, tildrakizumab
These therapies are primarily used to treat psoriasis, psoriatic arthritis, and other autoimmune skin disorders, improving both symptoms and overall well-being.
4. How Biologics Work
Biologics act by selectively interrupting specific immune pathways that drive autoimmune responses. For instance, TNF-alpha inhibitors block TNF-alpha, a protein that promotes inflammation, while IL-17 and IL-23 inhibitors target interleukins that play key roles in the inflammatory process. This targeted approach helps control disease activity with precision.
5. Benefits of Biologics
Patients often experience dramatic improvements, including reduced inflammation, clearer skin, decreased pain, and enhanced quality of life. Biologics can provide relief where traditional therapies have been insufficient, offering long-term management of chronic autoimmune conditions.
6. Risks and Side Effects
Because biologics suppress the immune system, there is an increased risk of infections. Common side effects include upper respiratory infections, injection site reactions, and allergic responses. Though rare, serious complications can include opportunistic infections and certain types of cancer.
7. Monitoring and Management
Regular monitoring is essential for patients receiving biologics. Physicians frequently evaluate for signs of infection and other potential side effects, often supplemented with routine blood tests to ensure safe and effective treatment.
| Biologic Class | Examples | Common Use |
| TNF-alpha Inhibitors | Etanercept, Adalimumab, Infliximab | Psoriasis, Psoriatic Arthritis |
| IL-17 Inhibitors | Secukinumab, Ixekizumab | Psoriasis |
| IL-23 Inhibitors | Guselkumab, Tildrakizumab | Psoriasis |
The Role of Biologics in Managing Autoimmune Conditions
Biologics have transformed autoimmune disease management by offering therapies that target immune dysfunction. This precision reduces symptoms, prevents tissue damage, and improves patients’ overall quality of life.
1. Understanding Biologics
Biologics are complex medications derived from living organisms, including monoclonal antibodies, recombinant proteins, and fusion proteins. Unlike chemically synthesized drugs, biologics are engineered to precisely target immune system components involved in autoimmune disease.
2. Mechanism of Action
These therapies work by selectively blocking or modulating overactive immune pathways. TNF-alpha inhibitors block a key inflammatory cytokine, while IL-6 inhibitors and B-cell depleters prevent immune overactivation. This targeted modulation reduces inflammation and prevents damage to affected tissues.
3. Common Autoimmune Diseases Treated with Biologics
Biologics are prescribed for a wide range of autoimmune diseases, including rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriasis, and multiple sclerosis. They can alleviate symptoms, reduce disease activity, and prevent long-term complications.
4. Types of Biologics
Available biologics include:
-
TNF-alpha inhibitors: Adalimumab, infliximab
-
IL-6 inhibitors: Tocilizumab
-
B-cell depleters: Rituximab
-
T-cell modulators: Abatacept
Choice depends on the specific disease, severity, and patient characteristics.
5. Efficacy and Benefits
Clinical trials demonstrate that biologics effectively reduce symptoms, prevent joint damage, and improve overall function. Many patients experience substantial relief, particularly when traditional therapies are insufficient.
6. Risks and Side Effects
While generally well-tolerated, biologics can increase susceptibility to infections. Side effects may include injection site reactions, respiratory infections, and rare serious complications like infusion reactions or certain cancers.
Effective Home Remedies for Itchy and Dry Scalp
Home-based treatments can provide relief for dry, itchy scalp:
-
Oils: Coconut, olive, or jojoba oil hydrate and soothe.
-
Apple Cider Vinegar: Balances scalp pH and reduces yeast overgrowth.
-
Aloe Vera: Offers anti-inflammatory relief.
-
Oatmeal Mask: Moisturizes and reduces irritation.
-
Tea Tree Oil: Provides antifungal and antibacterial benefits when used with a carrier oil.
Exploring Biosimilars in Autoimmune Therapy
Biosimilars are cost-effective alternatives to biologics, providing comparable safety and efficacy while expanding access for patients.
1. Understanding Biosimilars
Biosimilars are highly similar to approved biologics but are not generics. They demonstrate no clinically meaningful differences in safety, purity, or potency compared to the original product.
2. Biosimilars in Treatment
Biosimilars targeting TNF-alpha are effective in treating rheumatoid arthritis, Crohn’s disease, and psoriasis, showing results comparable to reference biologics.
3. Cost-Effectiveness
Lower cost enhances accessibility for patients who might otherwise be unable to afford biologic therapies, making them an important tool in healthcare management.
4. Considerations
Immunogenicity is a potential concern, though risk is low. Switching between reference biologics and biosimilars is generally safe under medical supervision.
Innovative Approaches in Autoimmune Disease Management
Emerging therapies improve precision and personalization in care.
1. Targeted Biologics and Immunomodulators
Newer biologics precisely target immune pathways, reducing off-target effects. Examples include IL-17 inhibitors for psoriasis and TNF inhibitors for rheumatoid arthritis.
2. Cell-Based Therapies
CAR-T therapy and stem cell transplants aim to reset or replace immune function, offering potential long-term remission in severe autoimmune diseases.
3. Nanotechnology and Drug Delivery
Nanoparticles enhance targeted delivery of medications, protect drugs from degradation, and improve bioavailability, minimizing systemic exposure and side effects.
Q&A
What are autoimmune diseases, and how do they affect the skin? Autoimmune diseases involve the immune system attacking the body, producing conditions like psoriasis, lupus, scleroderma, and dermatomyositis.
How do biologics treat autoimmune skin conditions? Biologics target immune components like TNF-alpha or interleukins to reduce inflammation and control disease activity.
Types, benefits, and risks of biologics? TNF-alpha, IL-17, and IL-23 inhibitors improve skin and quality of life but may increase infection risk.
Difference between biologics and biosimilars? Biologics are original therapies; biosimilars are highly similar, lower-cost alternatives with comparable efficacy.
References
https://www.numberanalytics.com/blog/ultimate-guide-biologics-autoimmune-skin-diseases
https://www.uspharmacist.com/article/the-expanding-role-of-biosimilars-in-autoimmune-diseases
https://www.autoimmuneinstitute.org
https://www.numberanalytics.com/blog/biologics-for-autoimmune-skin-diseases
https://ameripharmaspecialty.com/ivig/ivig-and-autoimmune-diseases/
How do you like this article?




